What is Leptospirosis?
Leptospirosis (synonyms: Vasiliev-Weil’s disease, infectious jaundice, nanakaya, Japanese 7-day fever, water fever, rest-meadow fever, fever of the meadow-fever, etc.) is an acute infectious disease caused by various types of women who have aphidpidor. general intoxication, damage to the kidneys, liver, nervous system. In severe cases, jaundice, hemorrhagic syndrome, acute renal failure and meningitis are observed.
Causes of Leptospirosis
The causative agent refers to the genus Leptospira, which includes only one species of Leptospira interrogate. The species is divided into two complexes – parasitic (Interrogans) and saprophytic (Biflexa). In each complex, serotypes (serological variants) are distinguished by antigenic properties; currently, about 200 pathogenic serotypes and about 60 saprophytic ones are known. Serotypes with common antigens are combined into serological groups. Pathogenic serotypes are combined into 23 serogroups. Separate serogroups are designated as follows, for example: Rotop’s serogroup of the species L. interrogans or L. interrgans var. rotop, but not L. roton.
Leptospirae have a spiral shape, have a straight and rotational mobility. In liquid media, leptospira is characterized by rotation around the long axis, dividing cells abruptly bend at the point of intended division. Leptospira are able to move in the direction of the medium with greater viscosity. The ends of leptospira are crooked in the form of hooks, but there may be hookless variants. The length of leptospira is 6–20 µm, and the diameter is 0.1–0.15 µm. The number of curls depends on the length (about 20 on average). Leptospira cultivated on media containing serum.
Leptospira are hydrophiles. An important condition for their survival in the environment is increased humidity and pH in the range of 7.0-7.4, the optimal growth of leptospira is observed at a temperature of 28-30 °C. Leptospira grow slowly, their growth is detected on the 5-7th day. A distinctive feature of saprophytic leptospira strains is their growth at 13 °C.
In our country, leptospira were isolated 13 serological groups, 27 serotypes. In particular, the following serogroups were distinguished: Rotop, Hebdomadis, Grippotyphosa, Canicola, Tarasovi.
Epidemiology. Leptospirosis is considered the most common zoonosis in the world. It is found on all continents except Antarctica, especially widespread in tropical countries.
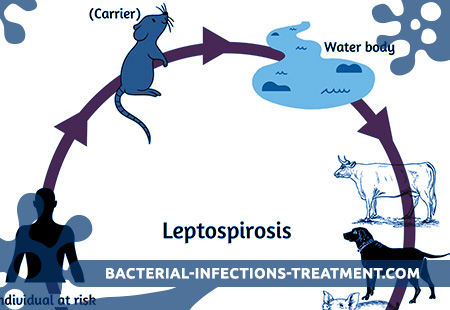
Sources of infection are various animals (forest mouse, vole, water rats, shrews, rats, dogs, pigs, cattle, etc.). A person with leptospirosis is not a source of infection. Transmission of infection in animals occurs through water and feed. Human infection most often occurs when skin and mucous membranes come into contact with water contaminated with animal secretions. It is important to contact with wet soil, as well as the slaughter of infected animals, cutting meat, as well as the use of certain products (milk, etc.) contaminated by secretions of infected rodents. Diseases often have a professional nature. Deratizers, people working in marshy meadows, workers in livestock farms, slaughterhouses, milkmaids, herders, veterinarians often fall ill. Leptospirosis is characterized by pronounced seasonality with a maximum incidence in August.
Pathogenesis during Leptospirosis
The gated infection is more often the skin. For the penetration of leptospiri sufficiently the slightest violation of the integrity of the skin. In this regard, infection occurs even with short-term contact with water containing leptospira. The pathogen can also penetrate through the mucous membranes of the digestive organs and conjunctiva of the eyes. There are no inflammatory changes (“primary affect”) at the site of the infection. Further promotion of leptospira occurs through the lymphatic ducts. Neither in lymphatic vessels, nor in regional lymph nodes, inflammatory events also develop. The barrier role of the lymph nodes is weak. Leptospira easily overcome them and entered into various organs and tissues (mainly in the liver, spleen, lungs, kidneys, central nervous system), in which reproduction and accumulation of leptospira occurs. By the time it coincides with the incubation period. This phase of pathogenesis equals the duration of the incubation period (from 4 to 14 days).
The onset of the disease (usually acute) is associated with a massive influx of leptospires and their toxins into the blood (microscopy reveals dozens of leptospirs in the field of view). The severity of the disease and the severity of organ lesions depends not only on the serotype of the pathogen, but also on the reactivity of the microorganism.
Secondary massive bacteremia leads to seeding of various organs, where the reproduction of pathogens continues. In victims of leptospirosis, there are numerous hemorrhages, the most intense in the area of skeletal muscles, kidneys, adrenal glands, liver, stomach, spleen and lungs. In the liver, leptospira are attached to the cell surface, and are also in the intercellular space. Part of leptospira dies. Leptospira, their toxins and metabolic products lead to severe intoxication, which increases especially quickly in the first 2-3 days from the onset of the disease. Leptospira have hemolysin, which leads to the destruction (hemolysis) of red blood cells. Pathogens and their toxic products have a pronounced effect on the vascular wall and blood coagulation system. In severe cases, thrombohemorrhagic syndrome develops.
Jaundice with leptospirosis is mixed. Hepatic tissue edema, destructive and necrotic changes of the parenchyma, as well as hemolysis of erythrocytes are important. Unlike viral hepatitis B, despite pronounced jaundice, acute hepatic failure develops rarely.
A special place in the pathogenesis of leptospirosis is renal damage. In most cases, deaths are associated with the development of acute renal failure (uremic coma). It occurs as a result of the direct action of leptospira and their toxic waste products on the cell wall, leading to severe damage to the epithelium of the renal tubules, cortical and subcortical substance of the kidneys, which leads to disruption of urinary processes. The consequence of this is oliguria with the possible development of uremia. In the genesis of anuria J, a significant reduction in blood pressure can also be significant, which is sometimes observed in leptospirosis. It is in the kidneys that leptospira are the most prolonged (up to 40 days).
In some patients (10-35%), leptospira overcome the blood-brain barrier, which leads to damage to the central nervous system, usually in the form of meningitis. Hemorrhages in the adrenal glands can lead to the development of acute insufficiency of the adrenal cortex.
A peculiar and pathognomonic manifestation of leptospirosis is the defeat of skeletal muscles (rhabdomialysis), especially expressed in the gastrocnemius muscles. Focal necrotic and necrobiotic changes typical for leptospirosis are found in the muscles. In biopsy specimens taken in the early stages of the disease, edema and vascularization are detected.
With the help of the immunofluorescence method, leptospirose antigen is detected in these foci. Healing occurs due to the formation of new myofibrils with minimal fibrosis. The breakdown of muscle tissue and damage to the liver lead to an increase in the activity of serum enzymes (AsAT, AlAT, alkaline phosphatase, etc.). Sometimes as a result of hematogenous drift, specific leptospirosis of the lungs (pneumonia), eyes (iritis, iridocyclitis), less often than other organs, develops.
In the process of the disease begins to form immunity. Before the introduction of antibiotics into patients with leptospirosis, antibodies appeared early and reached high titers (1: 1000-1: 100000), however, in recent years, with the early prescription of antibiotics, antibodies appear late (sometimes only during the recovery period and their titers are low). Immunity in leptospirosis is type-specific, that is, only in relation to the serotype that caused the disease. It is possible to re-infection with another leptospira serotype. The specific immunity is maintained for a long time.
In the period of early convalescence (usually after a 5-10-day apyrexia), a relapse of the disease is possible with the resumption of the main clinical manifestations of the disease. With adequate antibiotic therapy, relapses do not develop. In the process of recovery, the body is completely cleared of leptospira. Chronic forms of leptospirosis do not develop, although there may be residual effects, such as a decrease in vision after suffering leptospirosis iridocyclitis.
Symptoms of Leptospirosis
The incubation period lasts from 4 to 14 days (usually 7-9 days). The disease begins acutely, amidst full health without any precursors (prodromal phenomena). Chills appear, often severe, body temperature quickly reaches high numbers (39-40 ° C). Patients complain of severe headache, insomnia, lack of appetite, thirst. A very characteristic symptom is severe pain in the muscles, especially in the calf. The muscles of the thigh and lumbar region may be involved in the process, their palpation is very painful. In some patients, myalgia is accompanied by pronounced hyperesthesia of the skin (severe burning pain). Muscle pain is so severe that patients can hardly move or can not move at all (in severe forms).
An objective examination can be detected hyperemia and puffiness of the face, skin of the neck and upper chest (“hood symptom”) is also hyperemic. There is also an injection of the vessels of the sclera, but there are no signs of conjunctivitis (foreign body sensation in the eye, the presence of discharge, etc.). Body temperature is kept at a high level (fever usually of a permanent type) for 5-10 days, then decreases by short lysis. In some patients, especially if antibiotics were not prescribed, after 3-12 days, a second wave of fever is observed, which is usually shorter than the first. 2-3 relapses are very rare. In some patients after a decrease in body temperature a subfebrile condition is observed for a long time.
With a more severe course of leptospirosis, from the 3-5th day of the disease, the scleral icterus appears, and then the icteric staining of the skin, the severity of which varies widely (serum bilirubin can reach 200 µmol / l or more). At the same time, an exanthema appears in 20-50% of patients. Elements of the rash are polymorphic, located on the skin of the trunk and extremities. The rash may have a core-like, rubella-like, rarer scarlet-like character. Urtikar elements can also occur. Macular rash is prone to fusion of individual elements. In these cases, erythematous fields are formed. Erythematous rash is most common. With the development of hemorrhagic syndrome, petechial rash prevails. Often there is a herpetic rash (on the lips, nose wings). Thrombosis and hemorrhagic syndrome is manifested in addition to petechial rash hemorrhages into the skin at the injection sites, nosebleeds, hemorrhages in the sclera.
From the side of the cardiovascular system, bradycardia, hypotension, muffled heart sounds are observed, ECG shows signs of diffuse myocardial damage; in more severe forms, a detailed clinical picture of specific leptospirose myocarditis can be observed. In some patients develop moderate changes in the mucous membrane of the upper respiratory tract, most often in the form of rhinopharyngitis. Specific leptospirosis pneumonia is rarely observed. In almost all patients, by the 4th-5th day of the disease, an enlarged liver is observed, in half of the patients the spleen is enlarged. The liver is moderately painful on palpation.
In recent years, signs of central nervous system lesion in the form of pronounced meningeal syndrome (stiff neck, Kernig, Brudzinsky symptoms, etc.) have become more frequent (from 10–12% to 30–35%). In the study of cerebrospinal fluid, cytosis is noted (more often in the range of 400-500 cells in 1 μl) with a predominance of neutrophils. In some cases, the cerebrospinal fluid changes as with purulent meningitis with cytosis up to 3-4 thousand in 1 μl or more, with a predominance of neutrophils.
Most patients show signs of kidney damage. The amount of urine decreases sharply (before anuria). Protein appears in the urine (1 g / l or more), microscopy can detect hyaline and granular cylinders, renal epithelial cells. The blood increases the content of residual nitrogen, urea, creatinine. In case of severe disease, toxicosis increases, there may be signs of uremia (ulcers of the colon, humor friction noise, convulsions, disorders of consciousness up to the development of uremic coma). Acute renal failure is the main cause of death in patients with leptospirosis.
According to the clinical course, there are mild, moderate and severe forms of leptospirosis.
The manifestations characteristic of severe forms of leptospirosis are:
– development of jaundice;
– the appearance of signs of thrombohemorrhagic syndrome;
– acute renal failure;
– leptospirosis meningitis.
In this regard, severe forms of leptospirosis may be jaundiced (regardless of the serotype that caused the disease), hemorrhagic, renal, meningeal and mixed, in which there are two or more severity criteria. A disease characterized by high fever, severe intoxication, anemia and jaundice is sometimes referred to by the term “Weill syndrome”. In some patients, severe forms are characterized by the rapid development of acute renal failure without the occurrence of jaundice and hemorrhagic syndrome, and can end fatally at 3-5th day from the onset of the disease.
Moderate forms of leptospirosis are characterized by an expanded picture of the disease, severe fever, but without jaundice and other criteria for severe forms of leptospirosis.
Mild forms can occur with a 2-3-day fever (up to 38-39 ° C), moderate signs of general intoxication, but without pronounced organ lesions.
In the study of peripheral blood in the acute period of the disease observed neutrophilic leukocytosis (12-20×10 / 9l), increased ESR (up to 40-60 mm / h).
Complications of leptospirosis can be caused by leptospirae themselves, as well as by a stratified secondary bacterial infection. The first are meningitis, encephalitis, polyneuritis, myocarditis, iritis, iridocyclitis, uveitis. Pneumonia, otitis, pyelitis, and mumps are associated with the layering of secondary infection.
Complications that are observed only in children include increased blood pressure, cholecystitis, pancreatitis. A combination of manifestations such as myocarditis, hydropsy of the gallbladder, rash, redness and swelling of the palms and soles, followed by skin desquamating, fit into the picture of Kawasaki syndrome (Kawasaki disease). In recent years, complications have become more frequent.
Diagnosis of Leptospirosis
When recognizing leptospirosis, it is necessary to take into account the epidemiological background (profession, seasonality, contact with rodents, etc.) and characteristic symptoms. Differential diagnosis should be carried out depending on the clinical form and severity (predominance) of organ lesions. Severe icteric forms of leptospirosis have to be differentiated from viral hepatitis and icteric forms of other infectious diseases (pseudotuberculosis, infectious mononucleosis, salmonellosis, malaria, sepsis), less often with toxic hepatitis. In the presence of pronounced thrombohemorrhagic syndrome – with hemorrhagic fevers, sepsis, rickettsiosis. In renal failure – with hemorrhagic fever with renal syndrome. Mild forms of leptospirosis differentiate from influenza and other acute respiratory infections. When meningeal syndrome appears, it is necessary to differentiate both from serous meningitis (parotitis, enterovirus, tuberculosis, ornithosis, lymphocytic choriomeningitis) and from purulent (meningococcal, pneumococcal, streptococcal, etc.).
For laboratory confirmation of the diagnosis, data from conventional laboratory tests (neutrophilic leukocytosis, increased ESR, changes in urine, increase in the amount of bilirubin, residual nitrogen, etc.) are important. The most informative are specific methods. The diagnosis is confirmed by detection of a pathogen or an increase in the titer of specific antibodies. Leptospira in the first days of the disease can sometimes be detected in the blood using direct microscopy in a dark field, from 7-8 days you can microscopy the urine sediment, and with the appearance of meningeal symptoms and cerebrospinal fluid. However, this method often gives negative results (especially if the patient has already received antibiotics); This method often gives erroneous results, and therefore has not found wide application. The best results are obtained by sowing blood, urine, liquor. As a medium, you can use 5 ml of water with the addition of 0.5 ml of rabbit blood serum. In the absence of a medium, an anticoagulant should be added to the blood taken for the study (preferably sodium oxalate), and then leptospira last for about 10 days. You can use the infection of animals (hamsters, guinea pigs). The most common serological methods (RSK, microagglutination reaction). For the study take paired serum (the first to the 5-7th day of illness, the second – in 7-10 days). Positive are credits 1: 10-1: 20 and above. More reliable is the increase in antibody titers 4 times or more. With intensive antibiotic therapy, positive results of serological reactions sometimes appear late (after 30 or more days from the onset of the disease), and sometimes do not appear at all. Leptospira can be detected in gastrocnemius biopsy specimens (dyeing by silver plating). In dead, leptospira can be found in the kidneys and in the liver.
Leptospirosis Treatment
The main methods of treatment is the appointment of antibiotics and the introduction of a specific immunoglobulin. For the treatment of patients with severe forms of leptospirosis complicated by acute renal failure, pathogenetic therapy is of great importance. The most effective antibiotic is penicillin, in case of intolerance it can be used antibiotics tetracycline groups. The most effective treatment started in the initial period (up to the 4th day of illness). Penicillin is prescribed in a dose of 6,000,000-12,000,000 U / day, in severe forms that occur with meningeal syndrome, the dose is increased to 16,000,000-20,000,000 U / day. At the beginning of treatment with penicillin, the Jarish-Herxheimer reaction may develop during the first 4-6 hours. Of the tetracyclines, doxycycline is most effective (at a dose of 0.1 g, 2 times a day for 7 days). The drug is given orally. In severe general intoxication and hemorrhagic syndrome, antibiotics are combined with corticosteroid drugs (prednisone 40-60 mg with a gradual decrease in dose over 8-10 days).
Protivoleptospirozny immunoglobulin (gamma globulin) is administered after prior desensitization. On the first day, 0.1 ml of the diluted (1:10) immunoglobulin is injected under the skin, after 30 minutes, 0.7 ml of the diluted (1:10) immunoglobulin is injected under the skin and after another 30 min – 10 ml of the undiluted immunoglobulin intramuscularly. On the 2nd and 3rd days of treatment, 5 ml is administered (for severe forms, 10 ml each) of the undiluted immunoglobulin intramuscularly. Assign a complex of vitamins, symptomatic treatment. With the development of acute renal failure conduct a complex of appropriate therapeutic measures.
Forecast. The outcome of the disease depends on the severity of the clinical form. In the United States for 1974-1981 mortality averaged 7.1% (from 2.5 to 16.4%), with icteric forms it ranged from 15 to 48%, and for men over 50 years of age it was 56%.
Prevention of Leptospirosis
Protection of water sources from pollution. Stitched products from rodents.
Vaccination of animals. According to epidemiological indications, people may be vaccinated. Patients are not dangerous to others.