What is Diphtheria?
Diphtheria is an acute anthroponotic bacterial infection with general toxic phenomena and fibrinous inflammation at the entrance gate of the pathogen.
Brief historical information
The disease has been known since antiquity, Hippocrates, Homer, Galen mention it in their writings. Over the centuries, the name of the disease has repeatedly changed: “fatal ulcer of the pharynx”, “Syrian disease”, “hangman’s noose”, “malignant sore throat”, “croup”. In the XIX century P. Breton, and later his pupil A. Trusso presented a classical description of the disease, highlighting it as an independent nosological form called diphtheria, and then diphtheria (Greek diphthera – membrane, membrane).
E. Klebs (1883) found the pathogen in the films of the oropharynx, a year later F. Löffler isolated it in pure culture. A few years later, a specific diphtheria toxin was isolated (E. Ru and A. Yersen, 1888), antitoxin was detected in the patient’s blood and antitoxic anti-diphtheria serum was obtained (E. Ru, E. Bering, S. Kitazato, J.Y. Bardah, 1892 -1894). Its use has allowed to reduce mortality from diphtheria by 5-10 times. G. Ramon (1923) developed an anti-diphtheria toxoid. As a result of immunoprophylaxis, the incidence of diphtheria has drastically decreased; in many countries it was even eliminated.
In Ukraine, since the late 1970s, and especially in the 1990s, against the background of a decline in collective anti-toxic immunity, especially in the adult population, the incidence of diphtheria has increased. This situation was due to defects in vaccination and revaccination, a change in the biovars of the pathogen to more virulent and worsening socio-economic conditions of the population.
Causes of Diphtheria
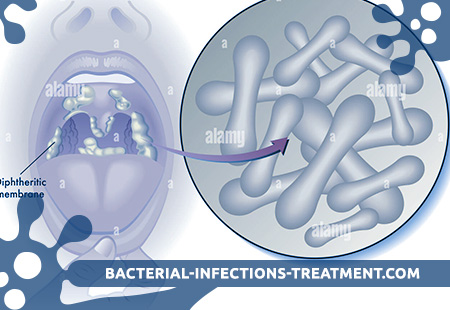
The causative agent of diphtheria is a gram-positive fixed rod-shaped bacterium Corynebacterium diphtheriae. Bacteria have club-shaped thickenings at the ends (Greek soguene – mace). When dividing, the cells diverge at an angle to each other, which determines their characteristic arrangement in the form of spread fingers, hieroglyphs, Latin letters V, Y, L, parquet, etc. Bacteria form volutin, the grains of which are located at the poles of the cell and are detected during staining. According to Naisser, the bacteria are stained brown-yellow with blue thickened ends. There are two main pathogen biovars (gravis and mitts), as well as a number of intermediate (intermedius, minimus, etc.). Bacteria are capricious and grow on serum and blood media. The most widely used media are tellurium (for example, Clauberg II medium), since the pathogen is resistant to a high concentration of potassium tellurite or sodium, which inhibits the growth of contaminating microflora. The main factor of pathogenicity is diphtheria exotoxin, attributed to highly active bacterial poisons. It is second only to botulinum and tetanus toxins. Only lysogenic strains of the pathogen infected with bacteriophage carrying the tox gene, encoding the structure of the toxin, exhibit the ability to toxin formation. Nontoxigenic strains of the pathogen are not capable of causing the disease. Adhesiveness, i.e. the ability to attach to the mucous membranes of the body and multiply, determines the virulence of the strain. The pathogen persists for a long time in the external environment (on the surface of objects and in dust – up to 2 months). Under the influence of a 10% solution of hydrogen peroxide, it dies after 3 minutes, while processing with a 1% solution of mercuric chloride, 5% solution of phenol, 50-60 ° ethyl alcohol – after 1 minute. Resistant to low temperature, when heated to 60 ° C dies after 10 min. Ultraviolet rays, chlorine-containing drugs, Lysol and other disinfectants also have an inactivating effect.
The reservoir and source of infection is a sick person or a carrier of toxigenic strains. The greatest role in the spread of infection belongs to patients with diphtheria of the oropharynx, especially with erased and atypical forms of the disease. Reconvalescents secrete the pathogen for 15–20 days (sometimes up to 3 months). Bacill carriers, which emit the pathogen from the nasopharynx, pose a great danger to others. In various groups, the long-term carrier rate varies from 13% to 29%. The continuity of the epidemic process provides a long-term carrier state even without registered morbidity.
The transmission mechanism is aerosol, the transmission route is airborne. Sometimes transmission factors can be contaminated hands and objects of the external environment (household items, toys, dishes, linens, etc.). Diphtheria of the skin, eyes, and genitals occurs when a pathogen is transported through contaminated hands. Also known food outbreaks diphtheria, due to reproduction of the pathogen in milk, pastry creams, etc.
The natural susceptibility of people is high and is determined by anti-toxic immunity. The content in the blood of 0.03 AE / ml of specific antibodies provides protection against the disease, but does not prevent the formation of a carrier of pathogenic pathogens. Diphtheria antitoxic antibodies transmitted by transplacental protect newborns from disease during the first half of their life. Antetoxic immunity is produced in people who have had diphtheria or correctly vaccinated people; its level is a reliable criterion of protection from this infection.
Major epidemiological signs. Diphtheria as a disease, depending on the inculcation of the population, according to WHO experts, can be successfully controlled. In Europe, extensive immunization programs began in the 1940s, and the incidence of diphtheria quickly declined to isolated cases in many countries. A significant decrease in the immune layer always accompanies the increase in the incidence of diphtheria. This happened in Ukraine in the early 90s, when, against the background of a sharp decline in collective immunity, there was an unprecedented rise in the incidence rate, especially of adults. Following an increase in the incidence of adults in the epidemic process, children who did not have antitoxic immunity were also involved, often as a result of unwarranted rejections from vaccinations. Migration in recent years has also contributed to the widespread pathogen. Periodic (in long-term dynamics) and autumn-winter (intra-annual) incidence rates are also observed with defects in vaccine prophylaxis. Under these conditions, the incidence may “shift” from a child to a more advanced age with a primary lesion of persons in threatened occupations (transport, trade, services, medical workers, teachers, etc.). A sharp deterioration in the epidemiological situation is accompanied by a more severe course of the disease and an increase in mortality. The rise in the incidence of diphtheria coincided with an increase in the circulation latitude of the biovars gravis and intermedius. Adults still prevail among the cases. Among vaccinated diphtheria flows easily and is not accompanied by complications. The introduction of infection into a somatic hospital is possible when the patient is hospitalized with a erased or atypical form of diphtheria, as well as a carrier of a toxigenic pathogen.
Pathogenesis during Diphtheria
The main entrance gate of the infection is the mucous membranes of the oropharynx, less often the nose and larynx, even less often the conjunctiva, ears, genitals, skin. Reproduction of the pathogen occurs in the area of the entrance gate. Toxigenic strains of bacteria secrete exotoxin and enzymes, causing the formation of a nidus of inflammation. The local effect of diphtheria toxin is expressed in coagulation necrosis of the epithelium, the development of vascular hyperemia and blood stasis in the capillaries, an increase in the permeability of the vascular walls. Exudate containing fibrinogen, white blood cells, macrophages and often red blood cells, goes beyond the limits of the vascular bed. On the surface of the mucous membrane as a result of contact with the thromboplastin of necrotic tissue, fibrinogen is converted into fibrin. The fibrin film is firmly fixed on the multilayered epithelium of the pharynx and pharynx, but is easily removed from the mucous membrane, covered with a single layer epithelium, in the larynx, trachea and bronchi. However, with a mild course of the disease, inflammatory changes may be limited only by a simple catarrhal process without the formation of fibrinous raids.
Neuraminidase of the pathogen significantly potentiates the action of exotoxin. The main part of it is histotoxin, which blocks protein synthesis in cells and inactivates the enzyme transferase, which is responsible for the formation of a polypeptide bond.
Diphtheria exotoxin spreads through the lymphatic and blood vessels, causing the development of intoxication, regional lymphadenitis and edema of the surrounding tissues. In severe cases, edema of the uvula, palatal handles and tonsils sharply narrows the entrance to the pharynx, edema of the cervical fat develops, the degree of which corresponds to the severity of the disease.
Toxinemia leads to the development of microcirculatory disorders and inflammatory and degenerative processes in various organs and systems – the cardiovascular and nervous systems, kidneys, adrenal glands. The binding of the toxin to specific cell receptors takes place in two phases – reversible and irreversible.
- In the reversible phase, cells retain their viability, and the toxin can be neutralized by antitoxic antibodies.
- In the irreversible phase, antibodies can no longer neutralize the toxin and do not interfere with the implementation of its cytopathogenic activity.
As a result, general toxic reactions and sensitization phenomena develop. In the pathogenesis of late complications of the nervous system, autoimmune mechanisms may play a role.
Antitoxic immunity, developing after suffering diphtheria, does not always protect against the possibility of recurrent disease. Anti-toxic antibodies have a protective effect in titers of at least 1:40.
Symptoms of Diphtheria
The incubation period lasts from 2 to 10 days. The clinical classification of diphtheria subdivides the disease into the following forms and course variants.
- Diphtheria of the oropharynx:
– oropharyngeal diphtheria localized with catarrhal, island and membrane variants;
– oropharyngeal diphtheria common;
– oropharyngeal subtoxic diphtheria;
– oropharyngeal diphtheria toxic (I, II and III degrees);
– diphtheria of the oropharynx is hypertoxic. - Diphtheria croup:
– laryngeal diphtheria (localized diphtheria croup);
– larynx and trachea diphtheria (croup widespread);
– diphtheria larynx, trachea and bronchi (descending croup). - Diphtheria nose.
- Diphtheria genitals.
- Diphtheria eye.
- Diphtheria skin.
- Combined forms with simultaneous damage to several organs.
Diphtheria of the oropharynx
Diphtheria of the oropharynx accounts for 90-95% of all cases of the disease in children and adults; in 70-75% of patients it occurs in a localized form. The disease begins acutely, increased body temperature from subfebrile to high persists for 2-3 days. Intoxication is moderate: headache, malaise, loss of appetite, pallor of the skin, tachycardia. With a decrease in body temperature, local manifestations in the area of the entrance gate persist and may even increase. The intensity of pain in the throat when swallowing corresponds to the nature of changes in the oropharynx, where dim congestive hyperemia is noted, moderate swelling of the tonsils, soft palate and arches are noted. The raids are localized only on the tonsils and do not extend beyond their borders, are located on separate islands or in the form of a film (insular or film variants). During the first hours of illness, fibrinous deposits look like a jelly-like mass, then – like a thin web-like film, but already on the 2nd day of the disease they become dense, smooth, grayish with a nacreous luster, are removed with difficulty, when they are removed with a spatula, the mucous membrane bleeds. The next day, a new film appears in place of the removed film. The removed fibrinous film placed in water does not break up and sinks. In the localized form of diphtheria, typical fibrinous deposits are observed in no more than 1/3 of adult patients, in other cases, as well as in later periods (3-5th day of illness), the attacks are loosened and removed easily, the bleeding of the mucous membrane during their removal is not expressed. Regional and submandibular lymph nodes are moderately enlarged and sensitive to palpation. The process on the tonsils and the reaction of the regional lymph nodes can be asymmetric or one-sided.
The catarrhal variant of the localized diphtheria of the oropharynx is rarely recorded, it is accompanied by minimal general and local symptoms. With normal or short-term subfebrile body temperature and weak manifestations of intoxication, there are unpleasant sensations in the throat when swallowing, a small hyperemia of the mucous membrane of the oropharynx, swelling of the tonsils. The diagnosis of diphtheria in such cases can be made only taking into account the history, the epidemic situation and the results of laboratory tests.
The course of localized diphtheria of the oropharynx is usually benign. After normalization, body temperature decreases and then the pain in the throat disappears, while the tonsils on the tonsils can persist for 6-8 days. However, if untreated, the localized form of oropharyngeal diphtheria may progress and move into other, more severe forms.
A common form of oropharyngeal diphtheria. They are relatively rare (3-11%). It differs from the localized form in the spread of attacks beyond the limits of the tonsils to any parts of the mucous membrane of the oropharynx. Symptoms of general intoxication, edema of the tonsils, pain in the submandibular lymph nodes are usually more pronounced than in the localized form. Edema of the subcutaneous tissue of the neck does not happen.
Subtoxic form of oropharyngeal diphtheria. Note the phenomena of intoxication, severe pain when swallowing, and sometimes in the neck. Tonsils purple-cyanotic color with a touch that is localized or slightly extending to the palatine arches and uvula. Swelling of the tonsils, arches, uvula and mild palate is moderate. Marked increase, tenderness and density of regional lymph nodes. A distinctive feature of this form is local edema of the subcutaneous tissue over the regional lymph nodes, often one-sided.
Toxic form of oropharyngeal diphtheria. Currently, they are encountered quite frequently (about 20% of the total number of patients), especially in adults. It can develop from an untreated localized or common form, but in most cases it occurs immediately and progresses rapidly. Body temperature is usually high (39-41 ° C) from the first hours of the disease. Note headache, weakness, severe pain in the throat, sometimes in the neck and abdomen. Vomiting, painful trism of masticatory muscles, euphoria, agitation, delirium, delirium may occur. Pale skin (with toxic diphtheria III degree, facial flushing is possible). Diffuse hyperemia and pronounced edema of the mucous membrane of the oropharynx, with toxic diphtheria II and III degrees, completely covering the lumen of the throat, precede the appearance of fibrinous deposits. The resulting raids quickly spread to all parts of the oropharynx. In the future, fibrin films become thicker and rougher, hold up to 2 weeks or more. The process is often one-sided. Regional lymph nodes grow early and significantly, become dense, painful, and periadenitis develops.
Local manifestations in toxic diphtheria of the oropharynx are distinguished from all other forms of the disease by the presence of painless, testicular edema of the subcutaneous tissue of the neck, which reaches its middle in toxic diphtheria of the I degree, and the clavicle – in the II degree. When grade III edema descends below the collarbone, can spread to the face, back of the neck, back and progresses rapidly.
General toxic syndrome is expressed, cyanosis of the lips, tachycardia, and lowering of arterial pressure are noted. With a decrease in body temperature, the symptoms remain pronounced. From the mouth of patients emanates a specific cloying-putrid odor, the voice acquires a nasal hue.
Toxic diphtheria of the oropharynx is often combined with lesions of the larynx and nose. Such combined forms are distinguished by a severe course, they are difficult to treat.
The hypertoxic form is the most severe manifestation of diphtheria. It develops more often in patients with an adverse premorbid background (alcoholism, diabetes, chronic hepatitis, etc.). The body temperature with a chill quickly increases to high numbers, intoxication is pronounced (weakness, headache, vomiting, dizziness, signs of encephalopathy). They note progressive hemodynamic disorders – tachycardia, weak pulse, low blood pressure, pallor, acrocyanosis. There are skin hemorrhages, organ hemorrhages, blood saturation of fibrinous raids, which reflects the development of DIC. The clinical picture is dominated by signs of a rapidly developing infectious-toxic shock, which can cause the death of a patient already on the 1-2 day of the disease.
Diphtheria croup
Allocate localized (diphtheria larynx) and common (with simultaneous lesion of the larynx, trachea and even the bronchi) forms. The common form is more often combined with diphtheria of the oropharynx, nose. Recently, this form of diphtheria is quite often met in adult patients. Clinically, croup is manifested in the form of three successively developing stages – dysphonic, stenotic and asphyxical – with moderately expressed intoxication phenomena.
- The leading symptoms of the dysphonic stage are a rough barking cough and increasing hoarseness. In children, it lasts 1-3 days, in adults – up to 7 days.
- During the stenotic stage (lasting from several hours to 3 days), the voice becomes aphonic, the cough is soundless. The patient is pale, restless, breathing is noisy, with a prolonged inhalation and drawing in of compliant areas of the chest. The increase in signs of difficulty breathing, cyanosis, tachycardia is considered as indications for intubation or tracheostomy, preventing the transition of diphtheria croup to the asphyxia stage.
- In the asphyxian stage, breathing becomes frequent and superficial, then rhythmic. Cyanosis increases, the pulse becomes filiform, blood pressure drops. In the future, consciousness is disturbed, convulsions appear, death from asphyxia occurs.
Due to the anatomical features of the larynx in adults, the development of diphtheria croup takes longer than in children, and there may be no involvement of the chest’s compliant places. In some cases, the only signs of this form of the disease are hoarseness and a feeling of lack of air. However, attention is drawn to the paleness of the skin, weakening of breathing, tachycardia, reduction of oxygen tension in the study of acid-base status. The laryngoscopic (in some cases, bronchoscopic) research that reveals hyperemia and edema of the larynx, films in the vocal cords, trachea and bronchi damage provides unconditional assistance in the diagnosis.
Diphtheria nose
Characterized by minor intoxication, difficulty in nasal breathing, sero-purulent or serous discharge (catarrhal variant). The mucous membrane of the nose is hyperemic, edematous, with erosions, ulcers, or fibrinous overlays in the form of easily removable “clumps” (foil variant). On the skin near the nose appear irritation, weeping and crusts. Diphtheria of the nose usually develops in combination with a lesion of the oropharynx and (or) larynx, sometimes the eye.
Diphtheria eye
It can occur in catarrhal, membranous and toxic variants.
In the case of a catarrhal variant, inflammation of the conjunctiva is noted (often one-sided) with non-abundant secretions. Body temperature is normal or low-grade. Symptoms of intoxication and regional lymphadenitis are absent.
With the foil variant, a fibrin film on the hyperemic conjunctiva forms on the background of subfebrile body temperature and weak general toxic effects, eyelid swelling increases, sero-purulent secretions appear. The process is at first one-sided, but after a few days it can go on to another eye.
Toxic diphtheria of the eyes has an acute onset, is characterized by the rapid development of symptoms of intoxication, eyelid edema, copious sukrovichno-purulent secretion, irritation and weeping of the skin around the eye. The edema spreads by capturing various areas of the subcutaneous tissue of the face. Laminated conjunctivitis is often accompanied by lesions of other parts of the eye, up to panophthalmia, as well as regional lymphadenitis.
Diphtheria of the ear, genitals (anal-genital), skin
These conditions are rarely met; they usually develop in combination with diphtheria of the throat or nose. The common features of these forms are edema, hyperemia, infiltration, fibrinous plaque in the affected area, regional lymphadenitis.
- In case of diphtheria of the genital organs in men, the process is localized in the region of the foreskin. In women, it can become common and seize the labia, vagina, perineum and the anus, accompanied by serous-bloody vaginal discharge, difficulty and painful urination.
- Diphtheria of the skin develops in the area of wounds, diaper rash, eczema, fungal lesions with cracked skin, where a scum of dirty-gray color with serous-purulent discharge is formed. General toxic effects are insignificant, however, the local process regresses slowly (up to 1 month or more).
The development of these forms contribute to the traumatization of the mucous membranes or skin, the drift of pathogens by hand.
In persons who have suffered diphtheria or have never had it, an asymptomatic carrier state can be observed, the duration of which varies significantly. Concomitant chronic diseases of the nasopharynx contribute to the formation of carriage. Antitoxic immunity does not prevent the development of carriage.
Complications
Pathogenetically caused complications of diphtheria include toxic shock, myocarditis, mono- and polyneuritis, including lesions of the cranial and peripheral nerves, polyradiculoneuropathy, adrenal lesions, toxic nephrosis. The frequency of their development in the localized form of diphtheria of the oropharynx is 5–20%, with more severe forms it increases significantly: in subtoxic diphtheria – up to 50% of cases, with varying degrees of toxic diphtheria – from 70 to 100%. The time of development of complications, counting from the onset of the disease, depends primarily on the clinical form of diphtheria and the severity of the process. Severe myocarditis, which is the most common complication of toxic diphtheria, occurs early – at the end of the first or beginning of the 2nd week of the disease. Moderate and mild myocarditis is detected later, at 2-3rd week. Toxic nephrosis as a frequent complication of only toxic diphtheria is detected by the results of urine tests already in the acute period of the disease. Manifestations of neuritis and polyradiculoneuropathy may occur both on the background of the clinical manifestations of the disease, and 2-3 months after recovery.
Diagnosis of Diphtheria
Differential diagnostics
Localized and widespread oropharyngeal diphtheria is differentiated with angina of various etiologies (cocci, Simanovsky-Vincent-Plaut’s sore throat, syphilitic, tularemia, etc.), infectious mononucleosis, Behcet’s syndrome, stomatitis. It is distinguished by moderate intoxication, pallor of the skin, soft hyperemia of the oropharynx, slow regression of manifestations of angina with a decrease in body temperature. With the foil variant, the fibrinous nature of the raids is much easier to diagnose. The most difficult for differential diagnosis is the islet variant of oropharyngeal diphtheria, often clinically indistinguishable from angina cocci etiology.
When making a diagnosis of toxic diphtheria of the oropharynx, it is necessary to carry out differential diagnostics with paratonsillar abscess, necrotic tonsillitis for blood diseases, candidiasis, chemical and thermal burns of the oral cavity. Toxic diphtheria of the oropharynx is characterized by rapidly spreading fibrinous deposits, swelling of the mucous membrane of the oropharynx and subcutaneous tissue of the neck, and pronounced and rapidly progressing manifestations of intoxication.
Diphtheria croup is differentiated from false croup in case of measles, ARVI and other diseases. The croup is often combined with diphtheria of the oropharynx or nose, clinically manifested in the form of three successively developing stages: dysphonic, stenotic, and asphyxian with moderately expressed intoxication phenomena.
Laboratory diagnosis
In the hemogram with a localized form of diphtheria, moderate, and with toxic forms, high leukocytosis, neutrophilia with a leukocyte shift to the left, an increase in ESR, and progressive thrombocytopenia are noted.
The basis of laboratory diagnosis is bacteriological studies: the isolation of the pathogen from the source of inflammation, the determination of its type and toxigenicity. The material is selected with sterile cotton swabs, dry or moistened (before sterilization!) With 5% glycerol solution. When storing and transporting tampons protect from cooling and drying. The material should be sown no later than 2-4 hours after collection. In patients with angina who have been in contact with patients with diphtheria, as well as in individuals with typical clinical manifestations of diphtheria, a diagnosis is made even with a negative result of bacteriological examination.
Auxiliary value is the determination of titers of anti-toxic antibodies in paired sera in the formulation of RNA. Toxin formation is detected using PhNG with an erythrocyte antibody diagnosticum. To identify diphtheria toxin proposed to use PCR.
Diphtheria treatment
All patients with diphtheria or with suspicion of it should be hospitalized. The duration of hospital stay and the length of bed rest depend on the form and severity of the disease. The main in the treatment of diphtheria is considered the introduction of antitoxic anti-diphtheria serum. It neutralizes the toxin circulating in the blood, therefore, has the greatest effect in early use. If you suspect a toxic form of diphtheria or diphtheria croup, serum is administered immediately, in other cases, waiting is possible with constant monitoring of the patient in the hospital. In patients with a localized form of diphtheria after the 4th day of illness, serum is tried not to be used, which, according to modern data, significantly reduces the possibility of developing long-term complications of the disease. The positive results of the skin test (Schick’s test) is a contraindication to the administration of serum only in localized forms, in all other cases in this situation the serum must be administered under the cover of antihistamines and glucocorticoids.
Anti-diphtheria serum can be administered either intramuscularly (more often) or intravenously. Repeated administration of serum is possible with continued intoxication. Currently, serum doses are being revised both upwards and downwards, depending on the form of diphtheria.
Conduct detoxification therapy with crystalloid and colloid solutions intravenously (polyionic solutions, glucose-potassium mixture with the addition of insulin, reopolyglukine, fresh frozen plasma). In severe cases, glucocorticoids (prednisone in a dose of 2-5 mg / kg) are added to the administered solutions. At the same time, these drip infusions contribute to the correction of hemodynamic disturbances. Used desensitizing drugs, vitamins (ascorbic acid, B vitamins, etc.).
Toxic diphtheria II and III degrees, hypertoxic form and severe combined forms of the disease – indications for plasmapheresis. Develop new effective ways of detoxification, such as hemosorption, affinity sorption, immunosorption.
In subtoxic and toxic forms, it is recommended to prescribe antibiotics that have an etiotropic effect on the concomitant cocci flora: penicillin, erythromycin, as well as ampicillin, ampiox, tetracycline preparations and cephalosporins in moderate therapeutic doses.
When diphtheria larynx requires frequent airing of the chamber, warm drinking, steam inhalation with chamomile, soda, eucalyptus, hydrocortisone (125 mg per inhalation). Patients prescribed aminophylline, saluretiki, antihistamines, with an increase in the phenomena of stenosis – prednisone intravenously at 2-5 mg / kg / day. In cases of hypoxia, humidified oxygen is used through a nasal catheter; films are removed using an electric suction device.
Indications for surgery – progression of signs of respiratory failure: tachypnea more than 40 per minute, cyanosis, tachycardia, motor restlessness, hypoxemia, hypercapnia, respiratory acidosis. In this case, with localized croup, tracheal intubation is performed, with widespread, descending croup and a combination of croup with severe forms of diphtheria — a tracheostomy with subsequent mechanical ventilation.
When signs of infectious-toxic shock occur, the patient is transferred to the intensive care unit. Along with active therapy by intravenous infusion of solutions, the dose of prednisone is increased to 5–20 mg / kg. In addition, dopamine (200–400 mg in 400 ml of 10% glucose solution intravenously at a rate of 5–8 ml / kg / min), trental (2 mg / kg intravenously in 50 ml of 10% glucose solution), trasylol or contrarikal (up to 2000-5000 IU / kg / day intravenously drip), saluretiki, izadrin.
Clindamycin 150 mg 4 times a day, benzylpenicillin-novocaine salt, 600 000 U, 2 times a day intramuscularly, and cefalotin and cephaleandol parenterally in medium therapeutic doses are used to rehabilitate the bacteria secrets. Course duration 7 days. It is advisable to simultaneously treat chronic pathology of upper respiratory tract.
Diphtheria Prevention
Epidemiological surveillance involves gathering information on the basis of which appropriate preventive measures can be taken. It includes not only the observation of the incidence and coverage of vaccination, but also the study of the immunological structure of the population, observation of the circulation of the pathogen among the population, its biological properties and antigenic structure. Of great importance are the epidemiological analysis and assessment of the effectiveness of the measures taken, and the prediction of the intensity of the epidemic process of diphtheria in a specific area.
Preventive actions
Vaccinal prophylaxis remains the primary method of controlling diphtheria. The immunization scheme for children involves immunization with DTP vaccine from 3 months of age (vaccinated 3 times with an interval of 30-40 days). Revaccination is carried out 9-12 months after the complete vaccination. For revaccination at 6–7, 11–12 and 16–17 years old, ADS-M is used. In some cases, such as contraindications to the pertussis component of DTP, ADS-M is also used for vaccination. In today’s epidemiological situation, the immunization of adults has become particularly important. Among adults, people at high risk are the first to be vaccinated:
- persons living in a dormitory;
- service workers;
- medical professionals;
- students;
- teachers;
- staff of schools, secondary and higher special institutions;
- workers of preschool institutions, etc.
ADS-M is used for vaccinations in adults in the form of routine immunization every 10 years to 56 years inclusive. Persons recovering from diphtheria are also subject to vaccinations. Diphtheria of any form in unvaccinated children and adolescents is regarded as the first vaccination, in those who received one vaccine before the disease – as the second vaccination. Further vaccinations are carried out according to the current vaccination schedule. Children and adolescents vaccinated against diphtheria (who have received a complete vaccination, one or more revaccinations) and have had a mild form of diphtheria without complications are not subject to additional vaccination after the disease. The next age revaccination is carried out in accordance with the intervals provided for by the current vaccination schedule.
Children and adolescents vaccinated against diphtheria (who have received a complete vaccination, one or more revaccinations) and who have had toxic forms of diphtheria should be vaccinated with the drug depending on age and health – once a dose of 0.5 ml, but not earlier than after 6 months after suffering the disease. Adults who have previously been vaccinated (who have received at least one vaccination) and have had mild diphtheria, are not eligible for additional vaccination against diphtheria. When they transfer the toxic form of diphtheria, they should be immunized against diphtheria, but not earlier than 6 months after the illness. Their revaccination should be carried out in 10 years. Persons with an unknown vaccination history are subject to serological screening for antitoxic antibodies. In the absence of a protective titer of antitoxins (more than 1:20), they are subject to vaccination.
The effectiveness of vaccination against diphtheria depends both on the quality of vaccine preparations and on the coverage of the population susceptible to the infection. A WHO-approved Expanded Program on Immunization states that only 95% immunization coverage ensures the effectiveness of vaccination.
The spread of diphtheria is prevented by early detection, isolation and treatment of patients and carriers of toxigenic diphtheria sticks. Of great preventive importance is the active identification of patients with diphtheria, providing for an annual routine examination of children and adolescents in the formation of organized groups. In order to detect early diphtheria, the local doctor (pediatrician, general practitioner) is obliged to actively monitor patients with sore throat with pathological impositions on the tonsils within 3 days from the initial treatment with obligatory bacteriological examination of diphtheria during the first day.
Activities in the epidemic focus
Patients with diphtheria should be hospitalized, and when hospitalization is delayed, they are urgently injected with 5000 IU of anti-diphtheria serum. Patients with severe forms of angina, patients from children’s institutions with the constant stay of children (children’s homes, orphanages, etc.), hostels living in adverse living conditions, persons belonging to the risk of diphtheria contingents (medical workers, employees of preschool institutions, health and educational institutions, workers of trade, public catering, transport), should be hospitalized with provisional purpose. Patients with a sore throat with raids or croup from a diphtheria focus are also hospitalized.
Discharge from the hospital is allowed after clinical recovery and a 2-fold negative result of bacteriological examination of mucus from the pharynx and nose for the presence of diphtheria pathogen, conducted at 2-day intervals, and not earlier than 3 days after the cancellation of antibiotic therapy. The discharge of the carrier of toxigenic diphtheria sticks is carried out after obtaining a 2-fold negative bacteriological examination result. After discharge from the hospital, patients and carriers of toxigenic diphtheria sticks are immediately allowed to work, study, and in children’s institutions with the constant stay of children without additional bacteriological examination. If the carrier of toxigenic diphtheria sticks continues to secrete the pathogen, despite the conduct of two courses of rehabilitation with antibiotics, it is allowed to work, study, and in preschool institutions. In these groups, all persons not previously vaccinated against diphtheria should be vaccinated according to the current immunization scheme. Only people vaccinated against diphtheria are again accepted into this group.
Diphtheria reconvalescents and carriers of diphtheria sticks are subject to follow-up within 3 months after discharge from the hospital. Clinical examination is carried out by the district therapist and the doctor of the office of infectious diseases in the clinic at the place of residence.
The doctor who established the diagnosis immediately sends an emergency notice to the Center for Sanitary and Epidemiological Surveillance. When isolating the source of infection, wet cleaning with the use of disinfectants, final disinfection of toys, bedding and linen are carried out. Bacteriological examination of those who communicated with the sick is carried out once. Only persons who have had direct contact with the patient or carrier of toxigenic strains of C. dyphtheriae are subject to serological examination in the outbreaks of diphtheria infection, in the absence of documentary evidence of their vaccination against diphtheria. Medical observation of them (including an otolaryngologist examination) is continued for 7 days. Identified patients and carriers of toxigenic diphtheria bacilli are hospitalized. Carriers of non-toxigenic strains cannot be treated with antimicrobial drugs, they are shown consultation of an otolaryngologist, identification and treatment of pathological processes in the nasopharynx. Not infected with diphtheria should be vaccinated in the focus of infection, as well as children and adolescents who have the next vaccination or revaccination period. Among adults, persons who, according to medical records, have passed 10 years or more, as well as people with low antibody titers (less than 1:20), are detected in adults for vaccination.